Melanoma
What is melanoma?
Melanoma is a life threatening malignant tumor that originates in cells called melanocytes, which are pigment-producing cells. The majority of melanomas are black or brown. However, some melanomas are skin-colored, pink, red, purple, blue or white.
Melanoma begins on the skin where it is easy to see and treat. However, it can grow into the skin, reaching the blood vessels and lymphatics, and can spread within the body to various organs when it can be fatal. If it is recognized and treated early, chances of recovery are very good. But if it is not found early, it can grow deeper into the skin, and spread to other parts of the body. Once melanoma spreads beyond the skin to other parts of the body, it becomes hard to treat and can be fatal.
The incidence of melanoma is increasing worldwide. The median age of diagnosis is 59 and the median age of death due to melanoma is 67.
Who is at risk for developing melanoma?
Everyone is at some risk for melanoma, but increased risk depends on several factors. These are sun exposure, number of moles on the skin, skin type and family history (genetics).
- Sun Exposure — Both UVA and UVB rays are dangerous to the skin, and can induce skin cancer, including melanoma. Blistering sunburns in early childhood increase risk, but cumulative exposure also is a factor.
- Moles — People with many moles are at an increase risk of developing melanoma. People with more than 50 moles are at a greater risk. Some people have irregular and unusual looking moles called atypical moles or dysplastic nevi. This increases the risk of melanoma.
- Family History — Any person who has a first-degree relative (mother, father, siblings or children) diagnosed with melanoma has a fifty percent greater chance of developing the melanoma than the person who does not have a family history of melanoma.
- Genetic risk — A mutation in the BRAF gene, may play a part in causing melanoma. Mutations in this gene can lead to uncontrolled cell growth and cancer. The mutations most commonly seen in familial melanoma occur in another gene, which is p53.
- Personal History — Person with a history of other type of skin cancer like basal cell carcinoma or squamous cell carcinomas are at increase risk for developing melanoma.
- Skin Type — Fairer skin is at increased risk of developing melanoma.
- Immune system — Any person with a compromised immune system has an increase chance to develop melanoma. The immune system can be compromised as a result of chemotherapy, HIV/AIDS or organ transplant.
How is melanoma diagnosed?
Moles, also called nevi, are groups of normal-appearing cells of melanocytic origin in the dermis. They are harmless brown spots on the skin. Melanoma usually looks different from the ordinary moles. The best way to find any suspicious moles on your body is to do a skin examination to look for the ABCDEs of melanoma. The first sign of melanoma is often a change in the size, shape, or color of a mole.
Melanoma also may appear as a new, black, abnormal or "ugly-looking" mole. Rarely, melanoma is not pigmented and is more difficult to diagnose. It may also appear as a non-healing ulcer or a new scar-like lump in the skin.
Melanoma checklist:
Examine yourself from head to toe and check for the following changes in your mole
| A |  |
ASYMMETRY | Half of the mole does not match the other half. |
| B |  |
BORDERS IRREGULARITY | The borders of the melanoma often are irregular or jagged. |
| C | 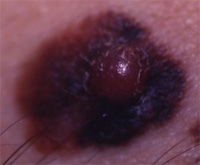 |
COLORS VARIEGATED | Having a variety of colors is a warning signal. The melanoma may have many shades throughout. Shades of brown, tan or black or also become red and blue color. |
| D | 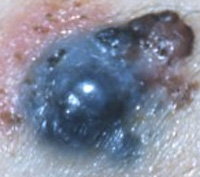 |
DIAMETER | Melanoma has a diameter of 6mm or more. |
| E |  |
EVOLUTION | There is a history of change in the lesion — size, shape, color, elevation or any symptoms such as bleeding, ulceration, itching or crusting. |
If you see one or more, make an appointment with a dermatologist immediately.
What are the different types of melanoma?
Melanomas fall into four basic categories.
- Superficial Spreading Melanoma — It is the most common type, accounting for about 70 percent of all cases. It is often seen in young people. In this type, melanoma travels along the top layer of the skin for a fairly long time before penetrating more deeply.
- Lentigo Maligna — This type of melanoma is found most often in the elderly, arising on chronically sun-exposed, damaged skin on the face, ears, arms and upper trunk.
- Acral lentiginous melanoma — It usually appears as a black or brown discoloration under the nails or on the soles of the feet or palms of the hands. It spreads superficially before penetrating more deeply. It is the most common melanoma in African-Americans and Asians, and the least common among Caucasians.
- Nodular Melanoma — It is usually invasive at the time it is first diagnosed. It is usually black, but occasionally is blue, gray, white, brown, tan, red or skin tone.
How is melanoma staged?
Melanoma is divided into 4 stages based on the depth of the primary tumor and how far the cancer has spread from its starting point. Melanoma staging system helps to identify the best treatment method for individual cases and also helps to identify the prognosis. In situ melanomas have an excellent prognosis after surgical excision with a sufficient surgical margin. Invasive melanomas are far more serious. Breslow thickness is the depth of the melanoma calculated perpendicularly from the skin surface, specifically from the stratum granulosum of the epidermis to the lower-most level of the melanoma (in mm).
What are the treatments available?
Early detection is the best treatment as it significantly increases the chances of survival. Any suspicious lesion should be immediately examined by a dermatologist who will then confirm the diagnosis by doing skin biopsy and looking for the presence of cancer cell under a microscope. Examination of the lesion under magnification with a dermoscope, before performing the biopsy has improved the clinical diagnosis of melanocytic lesion but does not replace the histopathology diagnosis. If melanoma is detected surgical excision of the entire lesion with surrounding normal tissue margin is usually the next first step.
-
Surgical Excision
Surgical excision is the first step in treatment for all stages of melanoma. Based on the pathological features of the tumor, it is removed completely along with surrounding normal tissue. This procedure reduces the chance of cancer cells being left behind. Margins for the excision is determined by the tumor invasion. This procedure is done using local anesthesia by a dermatologist or a surgeon as an outpatient procedure.
For invasive melanomas, it may require a sentinel lymph node biopsy. Sentinel lymph node biopsy is a procedure where a radioactive substance is injected near the melanoma. The first lymph node(s) to take up the substance is called the sentinel lymph node(s). (This imaging study is called lymphoscintigraphy). The surgeon removes the sentinel node(s) to check for cancer cells.
If the melanoma has spread to the nearby lymph nodes (sentinel lymph nodes), the affected lymph nodes are removed surgically. This procedure is called lymph node dissection where the surgeon removes all the lymph nodes in the area of melanoma.
-
Adjuvant Treatments
Usually, complete surgical excision of the melanoma is the only treatment needed for people with early-stage melanomas (thinner melanomas that have not spread to the lymph nodes) with regular follow-up visits with a dermatologist.
For late-stage melanomas (thick melanomas or those that have spread to the nearby lymph nodes), other treatments besides surgery may be needed. These are called "adjuvant" treatments, and they may take the form of:
- Chemotherapy — It uses substances similar to the ones that the body's immune system produces to destroy cancer cells. The two types of immunotherapy used for melanoma are interferon alpha and interleukin-2, which may be given after surgery for patients with metastatic melanoma or high risk of recurrence.
- Chemotherapy — It uses drugs to kill cancer cells. This is usually given in cycles whereby the treatment period is followed by a recovery period. Several chemotherapeutic agents have modest activity in melanoma. DTIC (dacarbazine) is the single most active agent in melanoma with the response rate of 15-20 %. Subcutaneous lesions, lymph nodes and pulmonary lesions are most likely to response to DTIC. Other drugs especially Cisplatin and Carmustine also have significant activity against melanoma.
- Radiation Therapy — It uses high energy rays to kill the cancer cells. It helps shrink the tumor and relieves the symptoms. It is used for advanced disease (stage IV) that has spread to brain, bones, or other organs.
Melanoma that has spread to distant sites in the body, such as the lungs or liver cannot be cured. In these cases, treatment usually focuses on relieving symptoms and keeping people as comfortable as possible.
People with advanced melanoma may be enrolled in clinical trials to try new and experimental treatment like interleukins, tumor necrosis factor, gene therapy, melanoma vaccines.
How can I prevent melanoma?
- Reducing Sun Exposure — The best way to prevent melanoma is to reduce the amount of time spend in the sun. Avoid sun between 10.a.m to 4 p.m.
- Wear Sun Protection and Protective Clothing — Apply generous amount of sunscreen to all the exposed area on the body, apply 20-30 minutes before sun exposure and reapply every two hours. Use a broad-spectrum sunscreen with sun protection factor of at least 15. Wear protective clothing, including long sleeves, long pants wide-brimmed hats, and sunglasses.
- Self-Skin Examination — From head to toe should be done every 6- 8 weeks, to look for any suspicious moles. It is important to always examine your skin to look for any changes in the moles (ABCDE's) or for development of new mole.
To learn more about melanoma and the clinical trials visit the following websites: